You Might Have More Than A Migraine If…
Occipital Headaches
Chiari headaches are felt at the occiput – at the base of the back of the skull and upper neck. They are generally tussive in nature, where they are exacerbated by valsalva maneuvers, which generally include: coughing, sneezing, heaving, laughing hard, or bearing down (like with a bowel movement or childbirth). These maneuvers reduce cardiac output (the amount of blood coming from the heart with each heartbeat), which in turn affects the attempted flow of cerebrospinal fluid, and it increases vagal stimuli. These headaches are often accompanied with feelings of vertigo, proprioception problems, gait problems, trouble swallowing, muscle spasms (commonly starts in the eyelids – blepharospasm), memory deficits, and cognitive difficulties (usually word recollection problems).

- For more on Chiari Malformation: http://chiaribridges.org//about-chiari/.
- For an expansive review of the name and definition of Chiari Malformation: http://chiaribridges.org//whats-in-a-name-chiari-malformation/.
Since the pushing down of the cerebellar tonsils can be congenital or acquired, we need to pay attention to other clues that our headaches might be indicating…
High-Pressure Headaches
Those that suffer from high pressure tend to feel pressure behind the eyes (often mistaken for sinus headaches) and report feeling like their “head is going to explode” from the pressure. High-pressure headaches are generally characterized by being worse when laying down – often awaking in the middle of the night or first thing in the morning with a headache, and the headache tends to dissipate to some degree after being upright for a period of time (and that period of time is different for everybody). Caffeine generally exacerbates high-pressure headaches.
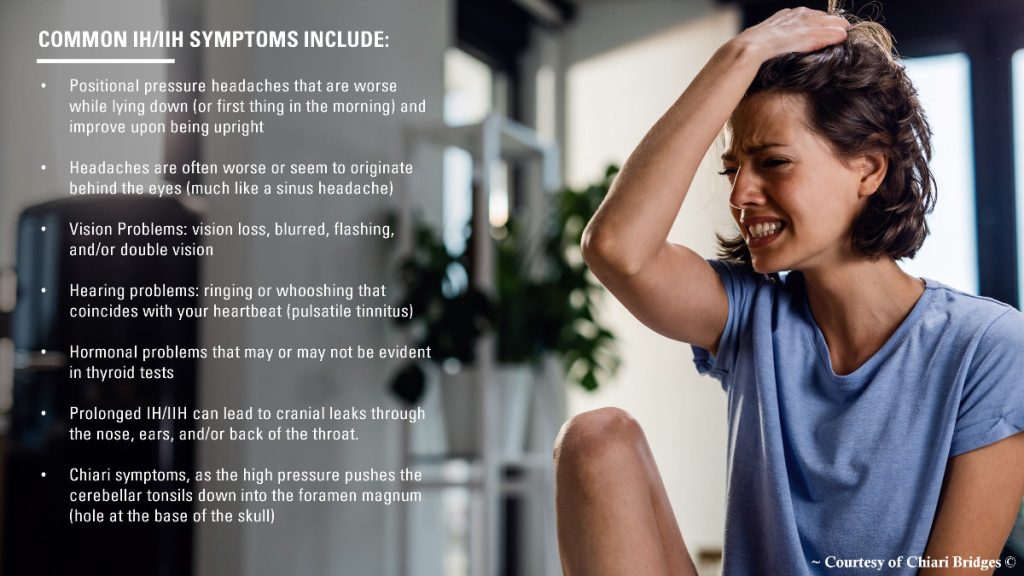
- For more on Intracranial HYPERtension: http://chiaribridges.org/brain-pressure-understanding-intracranial-hypertension/.
- For a list of common high-pressure symptoms:: http://chiaribridges.org//glossary/symptoms-of-intracranial-hypertension/.
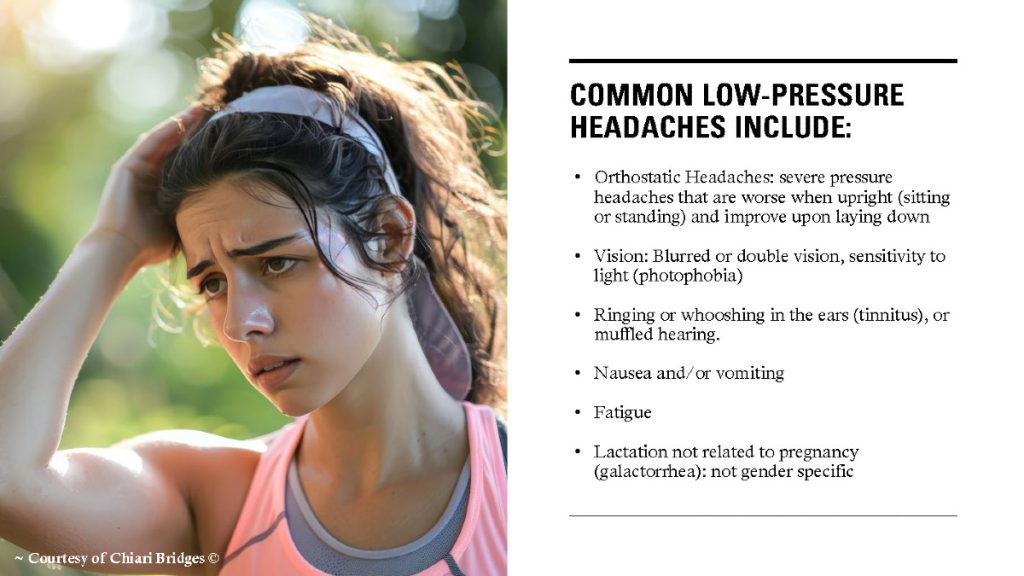
Low-Pressure Headaches
Those that suffer from low-pressure headaches tend to report feeling like there is an invisible pressure pushing down from the top of the head, often making it feel like your “head is going to implode.” Low-pressure headaches are characterized by being worse when upright and relieved by laying down. Low-pressure headaches are typically a sign of a cerebrospinal fluid leak (CSF Leak). The longer that the leak has existed, the less obvious the positional element is – meaning the patient can be upright longer before they feel the pressure at the top of their head, and they tend to need to lay down longer before getting any measure of relief. Caffeine often helps relieve low-pressure headaches.
- For more on Intracranial HYPOtension & CSF Leaks: http://chiaribridges.org//cerebrospinal-fluid-leaks/.
- For a list of common low-pressure symptoms:: http://chiaribridges.org//glossary/symptoms-of-intracranial-hypotension/.
Connecting the Three Headaches
- Untreated high pressure can cause cranial leaks (which leads to low pressure) – often accompanied by cerebrospinal fluid leaking through the nose or ears.
- CSF leaks can sometimes seal on their own leading to rebound high pressure (which is temporary) or continued high pressure if they originally had high pressure.
- Untreated high pressure can push the cerebellar tonsils down into the foramen magnum where it blocks the flow of cerebrospinal fluid, leading to occipital headaches (often diagnosed as a Chiari 1 Malformation) AND in return, the blockage of cerebrospinal fluid further increases intracranial pressure.
- Untreated low pressure can cause the brain to sag and as it sags the cerebellar tonsils can get lodged into the foramen magnum where it blocks the flow of cerebrospinal fluid, leading to occipital headaches (often diagnosed as a Chiari 1 Malformation).
- Untreated spinal leaks can create a suctioning or pulling down effect where the cerebellar tonsils can get lodged into the foramen magnum where it blocks the flow of cerebrospinal fluid, leading to occipital headaches (often diagnosed as a Chiari 1 Malformation).
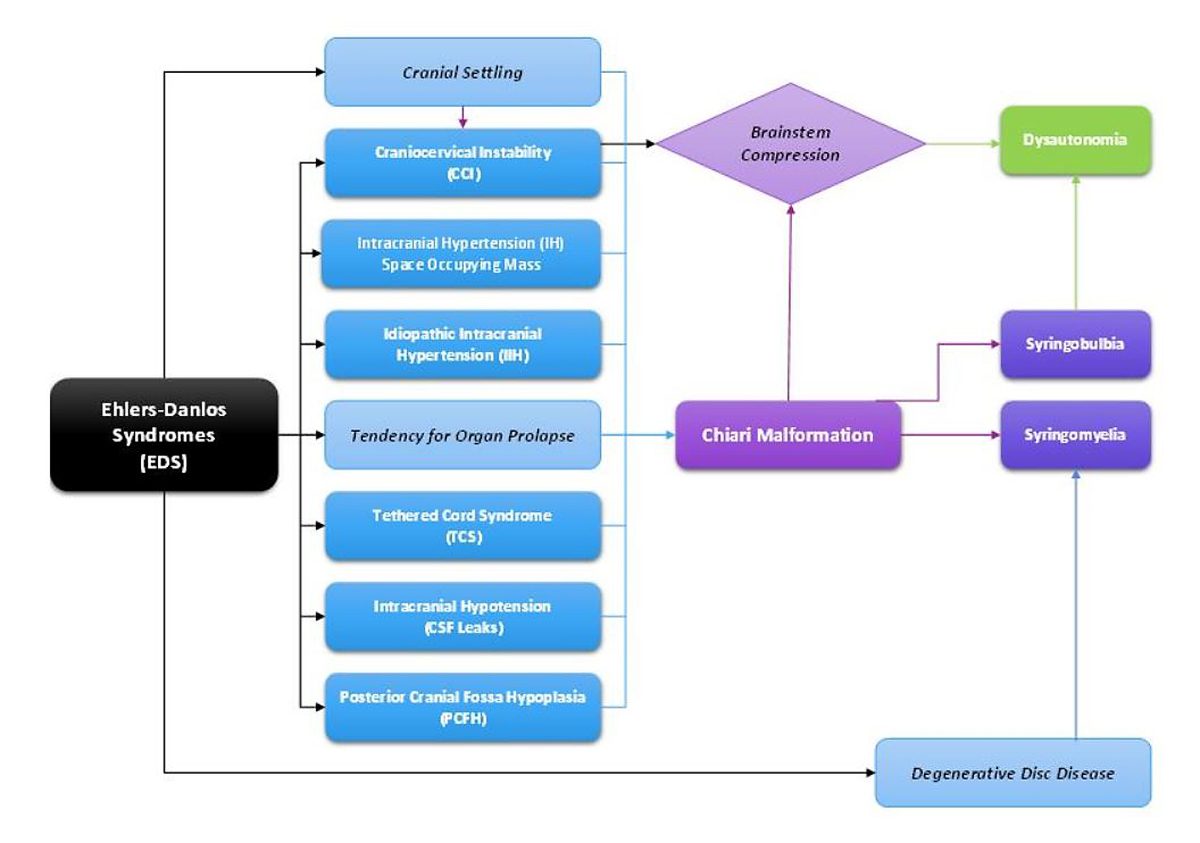
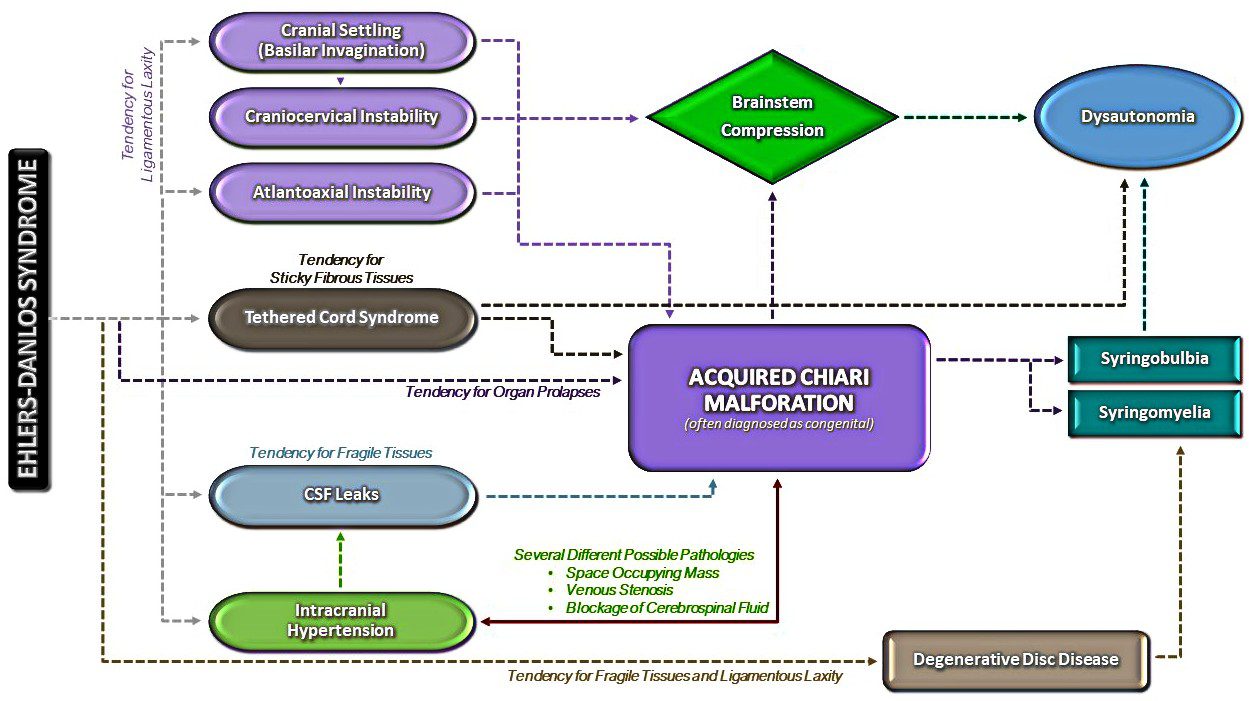
- All of the above is most common in patients with a connective tissue disorder such as Ehlers-Danlos Syndrome.

Major Problem Regarding Our Diagnoses & Treatment Options:
- Doctors and radiologists alike, tend to see the herniated tonsils and assume a small posterior fossa.
- Most do not check for high pressure or low pressure, even when directly asked and symptoms are present.
- When a posterior fossa decompression is finally offered, the high or low pressure is often left untreated which leads to a failed decompression.
- By the time sufferers get a name to go with their symptoms, we jump at the opportunity for relief.
The “Bobble-head Sensation” – When It Feels Like Your Neck Can No Longer Hold Up Your Head
While most of us experience this feeling either intermittently or continuously, it is generally related to structural instability issues:
- Craniocervical Instability (CCI, also known as Syndrome of Occipitoatlantialaxial Hypermobility) involves vertical hypermobility (back and forth sliding) of the craniocervical junction (interface between the occipital bone and the 1st and 2nd vertebrae), where the neck is no longer properly supporting the cranium. This condition can be dangerous as it often involves brain stem compression that can lead to a vast array of symptoms of Dysautonomia (dysfunction of the Autonomic Nervous System – ANS).

- For more on Craniocervical Instability and Other Related Disorders: http://chiaribridges.org/craniocervical-instability-related-disorders/.
- For a list of common CCI symptoms: http://chiaribridges.org//glossary/symptoms-of-craniocervical-instability/.
- For a list of common AAI (a condition commonly seen with CCI) symptoms: http://chiaribridges.org//glossary/symptoms-of-atlantoaxial-instability/.
- Subaxial Instability (SAI; also known as Cervical Instability) involves hypermobility of the C2/C3 to the C7 intervertebral discs. This condition (like most conditions involving the cervical spine) is a major cause of muscle spasms (in the neck and throughout the body at any point below the disc issues. When these neck spasms occur, they can cause the “Bobble-head sensation” where it feels like your neck can no longer hold up your head. This disc degeneration can lead to paralysis as discs compress the spinal cord.

Important Questions to Ask Your Neurosurgeons: http://chiaribridges.org/important-questions-for-your-neurosurgery-appointment/.
Originally written 10/2019
Updated 12/2022
Updated 11/2024