During my pregnancy I remember being very unwell, writing in my journal, “there is something wrong with pregnancy, I know something is wrong with my baby”, at only 10 weeks gestation; proving that a mother always knows. At around 30 weeks gestation my unborn baby started to get chronic hiccups followed by trembling, lasting several minutes and several times per day. I begged doctors to run further testing, pleading something was wrong but it all fell on deaf ears. Baby Eric’s heart rate was strong and steady, my fundus was measuring right on time with gestation, so my concerns were dismissed. At 36 weeks gestation, I started having consistent and lasting contractions. After several hours I proceeded to the ER department, concerned I was in preterm labor. Stress tests were run, and the nurses dismissed me, asking me to come back the next day for a follow up. While running a stress test the following day after food, juice and changing positions, the doctor was called as Eric didn’t have enough variables in his heart rate. I can still hear the Doctor yelling at the nurses asking why I had been sent home the night before demanding them to get on the phone with the hospital in the next community and to make sure a neonatal team was on standby, because they would be expecting a new Mom tonight. I was terrified, as all my worst fears were coming true. I was transported immediately, where I was met by a huge medical team. Everything was moving so quickly, myself and my partner were in shock and terrified not knowing what would come next. After an emergency ultrasound, Doctors explained that we had a very tiny baby with a great deal of amniotic fluid and something was seriously wrong with my baby; exclaiming that an emergency C-section would have to be performed. At this point we didn’t understand what this could mean, or why I had so much amniotic fluid. This was why my fundus was measuring well and everything went undetected. My partner and I were living every parent’s worst nightmare. Thinking back, I recall crying and holding my boyfriend’s hand as they carefully lifted a very tiny completely blue baby hand from my stomach. When we all saw my breathless baby like a flip of a switch the operating room became chaotic. Doctors were in a mad rush trying to resuscitate my baby, who had no vitals and wasn’t breathing. I was hysterical, so the doctors sedated me. My boyfriend was becoming increasingly agitated, so they demanded that he leave. I can still hear the nurses voice yelling at him, “you are taking up time we need to save your baby, you need to trust us and cooperate, OUT”, before the anesthesia flushed into my system.
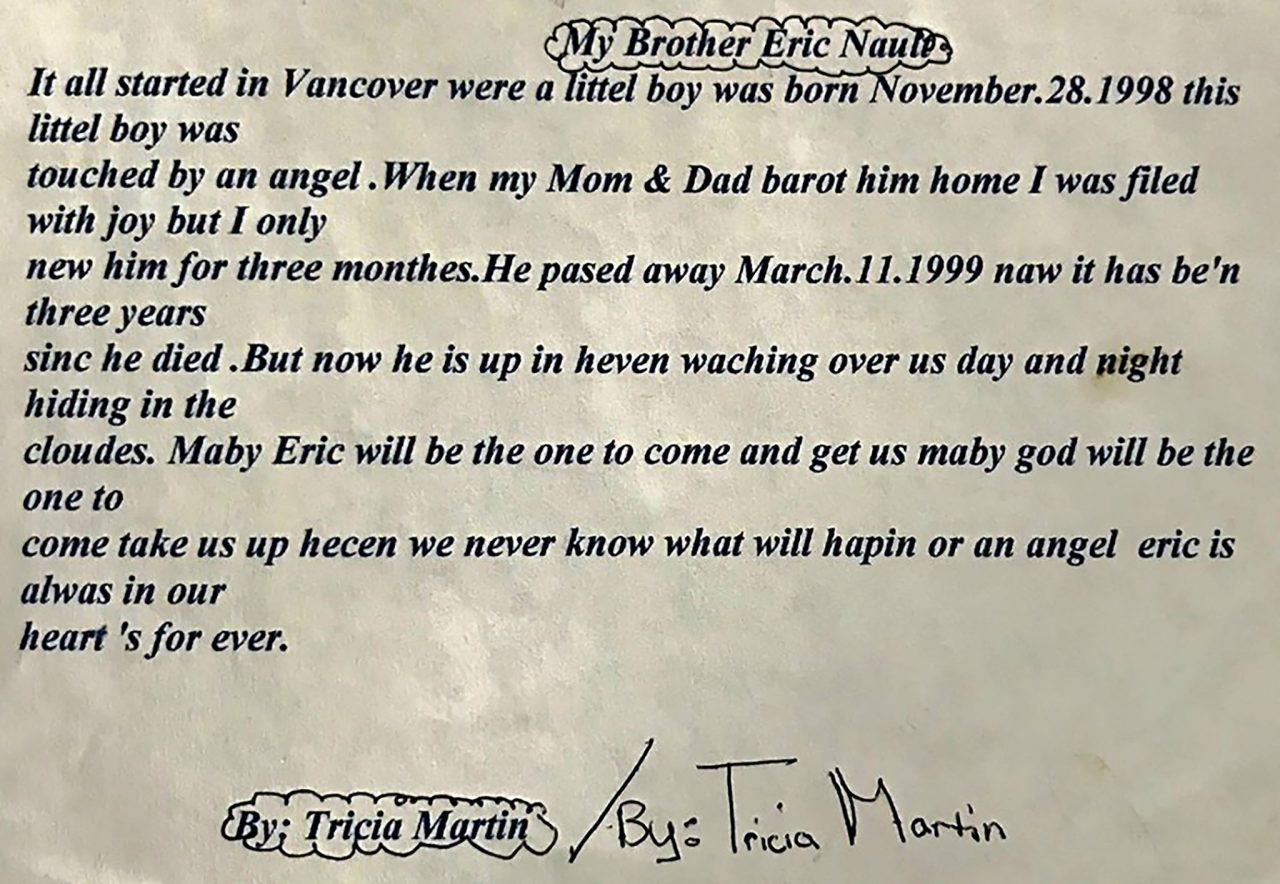
 After several hours I regained consciousness, family and doctors surrounded me trying to explain what they knew about baby Eric. They explained Eric and I would have to be immediately flown out to a larger center where they could properly care for my baby. Eric couldn’t support his own airway, he couldn’t suck, swallow, or move due to hypertonic muscles. He was having several seizures, all pointed to brain damage. At this point they had no idea what was wrong and could not conclude whether my baby would live. I recall saying I wanted to go see my baby and trying to get up out of the hospital bed, but the nurses told me I couldn’t see him, because I had just gone through a major surgery and he was too sick; we both had to rest for transport. When the nurses told me that, I flipped, telling them that come hell or high water, I was going to see him. I got as far as swinging my legs over the bed before I vomited everywhere. The nurses finally clued in that I was going with or without their help, so they laid me back down and wheeled me to the NICU to see him. I couldn’t even see my baby for he was so small and leads encased his body where he layed. They had his chin strapped up as every time it fell backward it would close off his airway leading to oxygen desaturation. They didn’t have the resources to intubate a baby at this hospital, so they decided to fly us out to Vancouver Children’s Hospital.
After several hours I regained consciousness, family and doctors surrounded me trying to explain what they knew about baby Eric. They explained Eric and I would have to be immediately flown out to a larger center where they could properly care for my baby. Eric couldn’t support his own airway, he couldn’t suck, swallow, or move due to hypertonic muscles. He was having several seizures, all pointed to brain damage. At this point they had no idea what was wrong and could not conclude whether my baby would live. I recall saying I wanted to go see my baby and trying to get up out of the hospital bed, but the nurses told me I couldn’t see him, because I had just gone through a major surgery and he was too sick; we both had to rest for transport. When the nurses told me that, I flipped, telling them that come hell or high water, I was going to see him. I got as far as swinging my legs over the bed before I vomited everywhere. The nurses finally clued in that I was going with or without their help, so they laid me back down and wheeled me to the NICU to see him. I couldn’t even see my baby for he was so small and leads encased his body where he layed. They had his chin strapped up as every time it fell backward it would close off his airway leading to oxygen desaturation. They didn’t have the resources to intubate a baby at this hospital, so they decided to fly us out to Vancouver Children’s Hospital.
The nurses and doctors kept me sedated for the first 4 days of being in Vancouver as every time I came to, I would start screaming for my baby and they would find me wandering the halls trying to find my baby. On day 4, they finally let my partner wheel me down to the NICU to see him. It was the scariest place I had ever seen. Rows and rows of incubators filled with tiny preemies with all kinds of machines keeping them alive. The nurse told me Eric was the biggest baby they had at 4 lbs. 11 oz. This gave me false hope, believing if he was bigger than all the others, he must have a fighting chance to survive. After several days of Eric in the NICU covered in wires, leads, and intubation tubes we still had no answers as to why our baby was born so ill. Eric was having up to 35 or more seizures per day, he was poked and prodded many times a day and underwent several tests; spinal taps, MRI’s, CT Scans and had several neonatal experts tirelessly working to find the cause of his many issues. Any parent who has been through this knows and understands the emotional roller coaster that comes with this experience. One day they tell you that your baby is improving, and they say he will beat this battle, and the next you’re told he wouldn’t survive the next 24 hours telling you to say your goodbyes; waking up all hours of the night, if you sleep at all, to pump your milk for a baby that isn’t there. You are walking to the hospital in the middle of the night just to be next to him because you can’t bear to be away. You are  begging, pleading to God for your child to be healed. After 3 weeks they finally let me have skin to skin cuddles and started teaching us how to care for him. This isn’t the way it’s supposed to go; you’re supposed to go to the hospital, have a baby and take them home, right? Instead you walk around numb, you don’t remember the last time you ate, or showered, you just feel like you’re having an out of body experience, as if you’re watching this happen to someone else. You’re scared to leave their side for even a minute because what if it’s that minute that he leaves this world and you’re not there?
begging, pleading to God for your child to be healed. After 3 weeks they finally let me have skin to skin cuddles and started teaching us how to care for him. This isn’t the way it’s supposed to go; you’re supposed to go to the hospital, have a baby and take them home, right? Instead you walk around numb, you don’t remember the last time you ate, or showered, you just feel like you’re having an out of body experience, as if you’re watching this happen to someone else. You’re scared to leave their side for even a minute because what if it’s that minute that he leaves this world and you’re not there?
We wouldn’t allow for anyone else to care for him, we did all his range of motion therapy, we did his bath time, and we did all his personal care alone because if a nurse or doctor touched him in a clinical manor he would be riddled with more seizures. After a month, the nurses started insisting we start taking better care of ourselves, so my boyfriend and I started alternating night shifts. My nights alone with him were my favorite, I would hold him all night and rock him. He would look up at me with his deep blue, soulful eyes and tell me all the secrets of the world. He had the oldest spirit I had ever saw, full of wisdom and love.
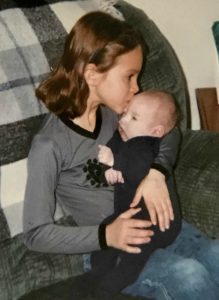
 After about a month we had a meeting, and it was then that the doctors told us we had a failure to thrive baby, his cells didn’t migrate to the right place at the right time, that his cerebellum and brainstem were severely underdeveloped. The statistics 19 years ago was that one out of one million babies were born like this and they had yet to find out what caused the illness. Our baby couldn’t regrow the parts of his brain that didn’t develop. He had gestational arrest at 32 weeks, he had scoliosis, spina bifida occulta, epilepsy and severe brain damage. Our child would never move on his own, suck or swallow or be able to interact and that he would most likely die of aspiration pneumonia. He would live his life in hospital more than out. I have worked with special needs adults with this type of quality of life, I could play the tape to the end, and I knew hanging on to him would only be for selfish reasons. I understood that my baby was in pain, I could see in his beautiful blue eyes, as I said before, a mother always knows. It was at this time Eric’s father and I decided to sign a” Do Not Resuscitate” order. It was without a doubt the single hardest thing I have ever done.
After about a month we had a meeting, and it was then that the doctors told us we had a failure to thrive baby, his cells didn’t migrate to the right place at the right time, that his cerebellum and brainstem were severely underdeveloped. The statistics 19 years ago was that one out of one million babies were born like this and they had yet to find out what caused the illness. Our baby couldn’t regrow the parts of his brain that didn’t develop. He had gestational arrest at 32 weeks, he had scoliosis, spina bifida occulta, epilepsy and severe brain damage. Our child would never move on his own, suck or swallow or be able to interact and that he would most likely die of aspiration pneumonia. He would live his life in hospital more than out. I have worked with special needs adults with this type of quality of life, I could play the tape to the end, and I knew hanging on to him would only be for selfish reasons. I understood that my baby was in pain, I could see in his beautiful blue eyes, as I said before, a mother always knows. It was at this time Eric’s father and I decided to sign a” Do Not Resuscitate” order. It was without a doubt the single hardest thing I have ever done.
We called our family to let them know of our decision and if they wanted an opportunity to say goodbye to Eric, they would have to travel down to do that as extubating was set for a week away. The doctors were certain he would pass away shortly thereafter. The family gathered, and we had our son baptized, pictures were taken, everyone had time alone to say what they needed to Eric, and he was extubated. Eric surprised us all; he just kept right on breathing, and he could support his airway after all. The hospital put us in a family room with our son, so we could spend as much time as we could with him in a less clinical environment before he passed.
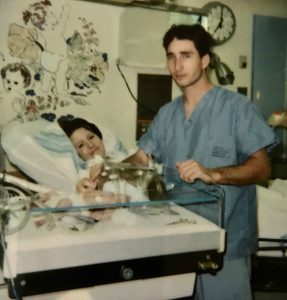
 Within 2 weeks, it was clear this child was a strong fighter and wasn’t ready to give up quite yet. We had another meeting and it was decided we would take him home. We wanted his big sister to have time with him and show him what a home was like. We took a 2-week crash course on neonatal nursing. We had to learn how to do his lung physio, how to suction him, and how to work a feeding pump and so much more. Eric was brought home February 10,1999. We did his 24-hour care until March 9th when he took a turn for the worse. He was diagnosed with aspiration pneumonia. This left me in a panic; I wasn’t ready to let him go, and I wanted him sent back to Children’s Hospital and be treated. We had an amazing Doctor who came to the hospital and took me for a walk to discuss why we made the DNR code and why we made the right choice for our son. I took my son home that day knowing we were running on borrowed time. His breathing became very shallow, he turned blue from lack of oxygen and on March 11, 1999 at 3:15 am our darling boy went home to be with his creator. The year following is a fog, I
Within 2 weeks, it was clear this child was a strong fighter and wasn’t ready to give up quite yet. We had another meeting and it was decided we would take him home. We wanted his big sister to have time with him and show him what a home was like. We took a 2-week crash course on neonatal nursing. We had to learn how to do his lung physio, how to suction him, and how to work a feeding pump and so much more. Eric was brought home February 10,1999. We did his 24-hour care until March 9th when he took a turn for the worse. He was diagnosed with aspiration pneumonia. This left me in a panic; I wasn’t ready to let him go, and I wanted him sent back to Children’s Hospital and be treated. We had an amazing Doctor who came to the hospital and took me for a walk to discuss why we made the DNR code and why we made the right choice for our son. I took my son home that day knowing we were running on borrowed time. His breathing became very shallow, he turned blue from lack of oxygen and on March 11, 1999 at 3:15 am our darling boy went home to be with his creator. The year following is a fog, I  remember very little. I was deeply depressed but I knew I had to keep moving forward for my daughter, she needed me. I know she was hurting too but I was so consumed with my own grief, that I couldn’t reach out to her, I couldn’t handle both her grief and mine. My daughter and I have had to take a lot of time since to heal together. With that being said, the pain of losing a child is not something that you can run away from or attempt to forget; I relive my sons small time on this earth every single day.
remember very little. I was deeply depressed but I knew I had to keep moving forward for my daughter, she needed me. I know she was hurting too but I was so consumed with my own grief, that I couldn’t reach out to her, I couldn’t handle both her grief and mine. My daughter and I have had to take a lot of time since to heal together. With that being said, the pain of losing a child is not something that you can run away from or attempt to forget; I relive my sons small time on this earth every single day.
Fast forward to 2005, I became very ill. It took 13 years for me to find out I had Chiari 1 Malformation and EDS and another 3 years too learn I too had Spina Bifida Occulta and Tethered Cord. I started to learn all I could on these conditions and joined many support groups. I was reading up on all the different types of Chiari when I came across Chiari Malformation type 4. It was described as one of the rarest types, when a baby is born with an underdeveloped hind brain or cerebellum. WHAT?! Did I just stumble across the reason as to why my son was born sick? Did I just stumble across the name of the disease that took my son from me? I printed out the info for Chiari 4 and Eric’s medical info and took it to my Doctor. The doctor and I had a long discussion and he agreed this was what my son had all those years ago, I just don’t think they called it Chiari 4 back in 1998. I was relieved to know, but angry. It took 18 years for me to find out what had happened to my darling baby and that was after all, genetic. They ran genetics on Eric but told us it was negative. Little did we know then that h-EDS was what I had and that they do not know the genes that cause it. I also learned many of us suffer from the MTHFR Gene where our bodies reject folic acid and B12, two vitamins I had always been deficient in and it can cause neural tube defects in babies.
In closing, I would like to say, no parent should have to wait 18 years to find out what took their child from them. As a parent, no matter how your child passes, you will blame yourself. I had to work through some pretty hard moments and learn to forgive myself for this unknown genetic disease that not only took my son Eric, but now has also made my oldest daughter Tricia ill. This is unacceptable to me. This is why it’s so important that we raise awareness and educate our doctors, so no mother or father has to wait 18 years to understand their child’s conditions or death. This is way the work that WTF and Chiari Bridges does is so very important to me and why I am always asserting that we be tested for all comorbid conditions. Rarely is Chiari just Chiari, so please take the time to undergo all the proper testing for all the comorbid conditions.

Eric Michael Nault November 28th, 1998 – March 11th, 1999.
Thank you for taking the time to remember my dear Eric with me,
Amy Schmalz



 I had a rough journey with these conditions and I am sharing it to help show how complex we can be and how much we need the medical community to step it up a notch (or ten)! I grew up in Denmark, where I lived when I was diagnosed and had my first surgeries.
I had a rough journey with these conditions and I am sharing it to help show how complex we can be and how much we need the medical community to step it up a notch (or ten)! I grew up in Denmark, where I lived when I was diagnosed and had my first surgeries.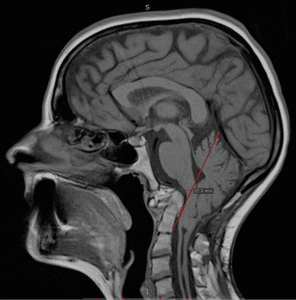 Years passed by with various periods of severe pain flares, flares that felt nothing like the pains I had before. But no doctor was really believing me. I had a spontaneous collapsed lung a couple of times in this period and ended up with surgery for this (I woke up under this surgery which later also turned out to have a significance). At 25, one day I had a sudden and severe onset of symptoms – a pain in the back of my head feeling like two stabbing knives. This did not resolve and after several attempts with various medicines, that I only got sicker from, I finally saw a new rheumatologist whom again treated me with harsh accusations of laziness and psychological imbalance. I can assure you he was the one bringing on my tears that day, despite the extra severe pain I had been in for weeks. I was placed in the care of the hospital physios and after a while, it became clear to them that there was something really wrong and they got me to see another rheumatologist, who in turn took their word and referred me for an MRI. I had only just turned 26 when I was diagnosed with Chiari 1 Malformation and Syringomyelia – in my full spine.
Years passed by with various periods of severe pain flares, flares that felt nothing like the pains I had before. But no doctor was really believing me. I had a spontaneous collapsed lung a couple of times in this period and ended up with surgery for this (I woke up under this surgery which later also turned out to have a significance). At 25, one day I had a sudden and severe onset of symptoms – a pain in the back of my head feeling like two stabbing knives. This did not resolve and after several attempts with various medicines, that I only got sicker from, I finally saw a new rheumatologist whom again treated me with harsh accusations of laziness and psychological imbalance. I can assure you he was the one bringing on my tears that day, despite the extra severe pain I had been in for weeks. I was placed in the care of the hospital physios and after a while, it became clear to them that there was something really wrong and they got me to see another rheumatologist, who in turn took their word and referred me for an MRI. I had only just turned 26 when I was diagnosed with Chiari 1 Malformation and Syringomyelia – in my full spine. I did a bit of internet research as information in Danish was very sparse and realized there was a certain number of bad outcomes due to something called Ehlers-Danlos Syndrome, Retroflexed Odontoid and Basilar Invagination. I asked my neurosurgeon, who was supposed to be the best in Denmark at this point, about these things – he claimed I didn’t have any. However, he did agree to refer me for Ehlers-Danlos evaluation. Here I was told I did not have that either. However, I was bordering on a similar connective tissue disorder called Marfan Syndrome, which they still could not diagnose me with due to my heart and eyes not being faulty. I had my first decompression surgery in December 2006. It was rough. I reacted badly to anesthetics and to the morphine and I also lost a lot of spinal fluid. I could not raise myself up the first month which I thought was normal. Slowly, I got better, and imaging showed my syrinx shrinking. Two and a half years later, though, I started experiencing dizziness and nausea and though my first surgeon didn’t believe me, imaging finally showed a big collection of fluid outside my spinal cord originating from a hole in the duraplasty used to close after tonsillar cauterization at my first surgery. I tried talking to the surgeon about concerns of Klippel-Feil and instability, that I had read about, but they would not hear of it and said that for now they would just focus on this issue. So, this was repaired, and I moved to Spain with my boyfriend at the time. I was placed on a disability pension from Denmark and that enrolled me in the Spanish public healthcare. I did, however, in the meantime follow up on my concerns and contacted a specialist, who had written about the Klippel-Feil and Chiari connection, and he straight away stated I had some severe issues with my odontoid and needed it removed and my neck fused to my skull. My first meeting with a surgeon in Spanish health care came up and he just looked at my imaging two minutes then stated my problems were way bigger than Chiari and Syringomyelia. He also diagnosed a severe retroflexed odontoid and Basilar Invagination – so severe he had a hard time understanding how I could breathe, let alone walk. But given my reasonably good condition, he opted to postpone these surgeries as they are big and not without risks.
I did a bit of internet research as information in Danish was very sparse and realized there was a certain number of bad outcomes due to something called Ehlers-Danlos Syndrome, Retroflexed Odontoid and Basilar Invagination. I asked my neurosurgeon, who was supposed to be the best in Denmark at this point, about these things – he claimed I didn’t have any. However, he did agree to refer me for Ehlers-Danlos evaluation. Here I was told I did not have that either. However, I was bordering on a similar connective tissue disorder called Marfan Syndrome, which they still could not diagnose me with due to my heart and eyes not being faulty. I had my first decompression surgery in December 2006. It was rough. I reacted badly to anesthetics and to the morphine and I also lost a lot of spinal fluid. I could not raise myself up the first month which I thought was normal. Slowly, I got better, and imaging showed my syrinx shrinking. Two and a half years later, though, I started experiencing dizziness and nausea and though my first surgeon didn’t believe me, imaging finally showed a big collection of fluid outside my spinal cord originating from a hole in the duraplasty used to close after tonsillar cauterization at my first surgery. I tried talking to the surgeon about concerns of Klippel-Feil and instability, that I had read about, but they would not hear of it and said that for now they would just focus on this issue. So, this was repaired, and I moved to Spain with my boyfriend at the time. I was placed on a disability pension from Denmark and that enrolled me in the Spanish public healthcare. I did, however, in the meantime follow up on my concerns and contacted a specialist, who had written about the Klippel-Feil and Chiari connection, and he straight away stated I had some severe issues with my odontoid and needed it removed and my neck fused to my skull. My first meeting with a surgeon in Spanish health care came up and he just looked at my imaging two minutes then stated my problems were way bigger than Chiari and Syringomyelia. He also diagnosed a severe retroflexed odontoid and Basilar Invagination – so severe he had a hard time understanding how I could breathe, let alone walk. But given my reasonably good condition, he opted to postpone these surgeries as they are big and not without risks. A couple of years of enjoying the benefits the climate change gave me (and likely putting my head in the sand) went by but then I could no longer ignore the fact that I was getting worse. I was in a rough period with other matters of life, so it took a while before I realized I couldn’t escape the changes in my body. I started losing weight amongst other things and after a quick detour of fear of stomach cancer, I finally realized that everything that was going on was related to my brainstem compression. So, I went back to the neurosurgeon. He ordered some testing but before it could be done, I ended up admitted urgently after I stopped breathing one night. From here started a roller coaster. I didn’t feel right about their suggestions and the surgeon that was going to operate didn’t feel very secure himself even. I ended up getting transferred to a private hospital in Barcelona that calls themselves a “Chiari Institute.” Had I known what I do now, I would never have paid the fee for a filum release, but the doctor claimed this was what I needed and well… It was worth a shot in this urgent situation. He then sent me home, claiming I was cured. I didn’t feel right and breathing through the night was still a problem, so I started sending my imaging to experts around the world and working on getting referred to another hospital in Spain’s public health with higher expertise. All these experts claimed I wouldn’t have long to live unless I had this odontoid approached.
A couple of years of enjoying the benefits the climate change gave me (and likely putting my head in the sand) went by but then I could no longer ignore the fact that I was getting worse. I was in a rough period with other matters of life, so it took a while before I realized I couldn’t escape the changes in my body. I started losing weight amongst other things and after a quick detour of fear of stomach cancer, I finally realized that everything that was going on was related to my brainstem compression. So, I went back to the neurosurgeon. He ordered some testing but before it could be done, I ended up admitted urgently after I stopped breathing one night. From here started a roller coaster. I didn’t feel right about their suggestions and the surgeon that was going to operate didn’t feel very secure himself even. I ended up getting transferred to a private hospital in Barcelona that calls themselves a “Chiari Institute.” Had I known what I do now, I would never have paid the fee for a filum release, but the doctor claimed this was what I needed and well… It was worth a shot in this urgent situation. He then sent me home, claiming I was cured. I didn’t feel right and breathing through the night was still a problem, so I started sending my imaging to experts around the world and working on getting referred to another hospital in Spain’s public health with higher expertise. All these experts claimed I wouldn’t have long to live unless I had this odontoid approached. October 2016 I finally had a partial odontoidectomy and a fusion, which beyond doubt saved my life. It was a rough ride, for both me and the surgeons. They had to deal with complications related to my anatomy, to the mess the first surgeon in Denmark had left – he had indeed damaged my muscles more than I ever knew – and to the problems relating to the soft tissue. I do know they did a great job, but due to all the mistakes, how complicated my case was and is, I am unfortunately not done. I have ongoing issues and though some of these could have been avoided with the right approach from the beginning, some are just the way it is with these conditions.
October 2016 I finally had a partial odontoidectomy and a fusion, which beyond doubt saved my life. It was a rough ride, for both me and the surgeons. They had to deal with complications related to my anatomy, to the mess the first surgeon in Denmark had left – he had indeed damaged my muscles more than I ever knew – and to the problems relating to the soft tissue. I do know they did a great job, but due to all the mistakes, how complicated my case was and is, I am unfortunately not done. I have ongoing issues and though some of these could have been avoided with the right approach from the beginning, some are just the way it is with these conditions.
 Zona McGee was blessed with a vibrant and beautiful little boy on July 2nd, 1993. She named him Ryan Andrew and fell in love with his sweet face the second she first held him. He looked just like her! Her husband, Kevin, and daughter Crystal, eight-years old at the time, were over the moon as well.
Zona McGee was blessed with a vibrant and beautiful little boy on July 2nd, 1993. She named him Ryan Andrew and fell in love with his sweet face the second she first held him. He looked just like her! Her husband, Kevin, and daughter Crystal, eight-years old at the time, were over the moon as well. Ryan was a good student and took a local job after graduating from high school. He loved working and earning his own money. By all accounts, Ryan was a completely normal, functioning, and on-target, young adult. He was doing what most recent high school grads do – living life, having fun, and trying to decide what profession he might go into.
Ryan was a good student and took a local job after graduating from high school. He loved working and earning his own money. By all accounts, Ryan was a completely normal, functioning, and on-target, young adult. He was doing what most recent high school grads do – living life, having fun, and trying to decide what profession he might go into. Over the next few months, Ryan was rushed to the E.R. on several occasions due to cyclic, intractable, vomiting along with severe head and neck pain. During these dozen-plus visits to the E.R., he was turned away multiple times and labeled “drug-seeking, weak, and dramatic.” This was a slap in the face, as Ryan was advised to blindly have the surgery to prevent him from returning to the E.R. This painful irony was not lost on Zona, and it only added to her trauma and confusion.
Over the next few months, Ryan was rushed to the E.R. on several occasions due to cyclic, intractable, vomiting along with severe head and neck pain. During these dozen-plus visits to the E.R., he was turned away multiple times and labeled “drug-seeking, weak, and dramatic.” This was a slap in the face, as Ryan was advised to blindly have the surgery to prevent him from returning to the E.R. This painful irony was not lost on Zona, and it only added to her trauma and confusion. On the last visit to this particular hospital, the chief neurosurgeon refused to treat him neurologically and ordered a psychiatric evaluation instead. After speaking with Ryan, the psychiatrist said, “I do not believe you are crazy, but you are a bit of a wimp.”
On the last visit to this particular hospital, the chief neurosurgeon refused to treat him neurologically and ordered a psychiatric evaluation instead. After speaking with Ryan, the psychiatrist said, “I do not believe you are crazy, but you are a bit of a wimp.”![The Christopher Ellington Story – A Chiari Warrior’s Journey [Updated]](https://chiaribridges.org/wp-content/uploads/2017/05/hosp1.jpg)

