- Connective Tissues
- The Importance of Collagen
- The Ehlers-Danlos Syndromes
- Affected Body Systems
- Affected Pathologies
Connective tissues provide strength and flexibility to structures such as bones, ligaments, muscles, organs, and blood vessels. Connective tissue problems typically involve a problem with one or more of the proteins.
There are over 200 identified Heritable Disorders of Connective Tissue (HDCTs),[2] conditions such as Marfan Syndrome, Loeys-Dietz Syndrome, Stickler Syndrome, Osteogenesis Imperfecta, Pseudoxanthoma Elasticum, and Epidermolysis bullosa - all involve one of the many proteins that make up our bodies connective tissues.
There are over 200 identified Heritable Disorders of Connective Tissue (HDCTs),[2] conditions such as Marfan Syndrome, Loeys-Dietz Syndrome, Stickler Syndrome, Osteogenesis Imperfecta, Pseudoxanthoma Elasticum, and Epidermolysis bullosa - all involve one of the many proteins that make up our bodies connective tissues.
Collagen makes up 30% of the proteins in the human body.
It is often likened to the “cellular glue that holds us together.”
Imagine the difference between something bonded together with Gorilla Glue versus watered down Elmer’s Glue. The creation using Elmer’s Glue wouldn’t be as strong. The consistency of Elmer’s Glue could cause anything depending on it to lose its form and then gravity will cause it to prolapse/herniate.
Just as our skin has collagen and as we age, we see the effects with sagging eyelids, cheeks and neck areas; our brains have collagen which helps them to keep their form. Your spine is a mass collection of vertebrae bound together by connective tissue and the protein that binds each disc together is collagen.
It is often likened to the “cellular glue that holds us together.”
Imagine the difference between something bonded together with Gorilla Glue versus watered down Elmer’s Glue. The creation using Elmer’s Glue wouldn’t be as strong. The consistency of Elmer’s Glue could cause anything depending on it to lose its form and then gravity will cause it to prolapse/herniate.
Just as our skin has collagen and as we age, we see the effects with sagging eyelids, cheeks and neck areas; our brains have collagen which helps them to keep their form. Your spine is a mass collection of vertebrae bound together by connective tissue and the protein that binds each disc together is collagen.
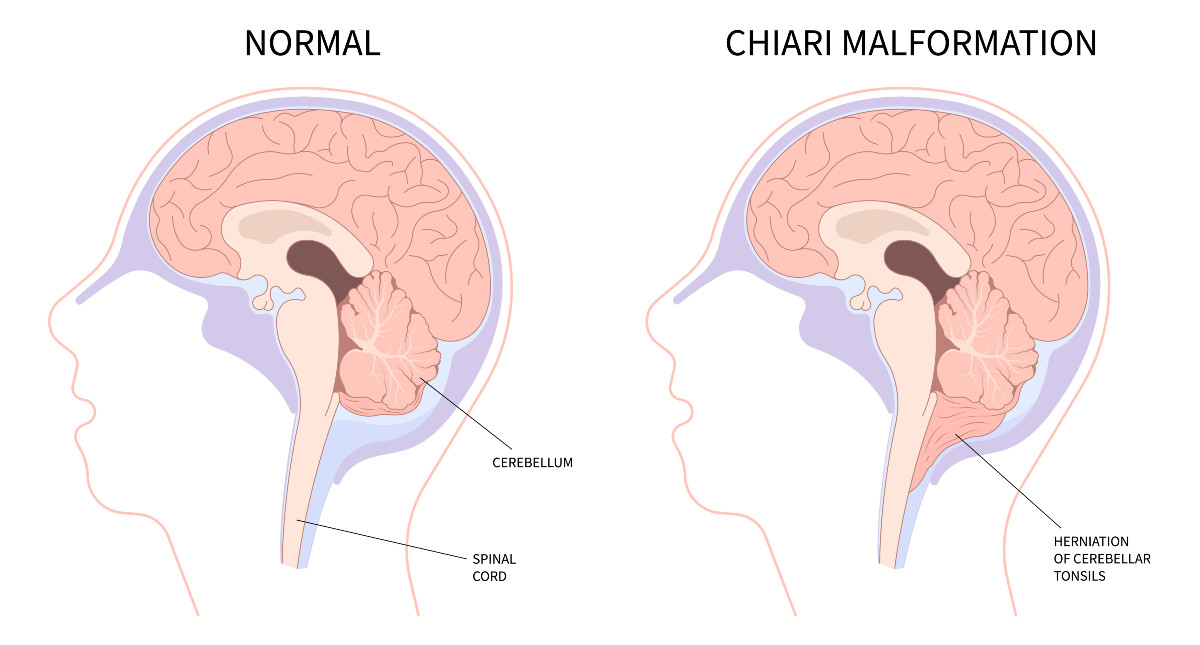
Contrary to popular belief, a Chiari Malformation does not indicate a large brain or a small skull. Most doctors ascribe to the belief that a Chiari Malformation is nothing but a congenitally underdeveloped posterior cranial fossa (posterior fossa hypoplasia) in fact, the surgical treatment that they recommend is technically called a Posterior Fossa Decompression (not a Chiari Decompression, as patients tend to call it).
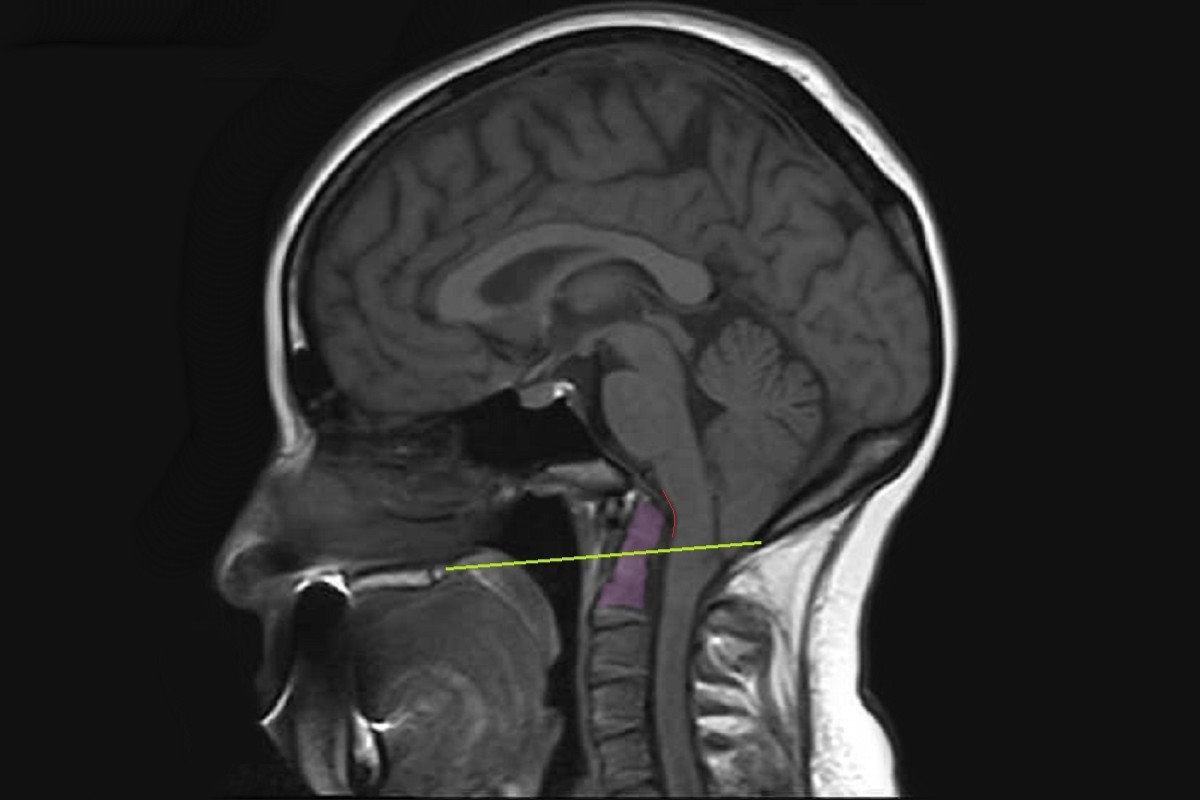
A small posterior fossa does not cause a problem unless it pushes the cerebellar tonsils down into the foramen magnum (the hole at the base of the skull), causing a blockage of cerebrospinal fluid. Yet, the size of that herniation is THE ONLY THING that doctors routinely measure when they diagnose a Chiari Malformation. They diagnose according to a criteria that only considers the size and appearance of the cerebellar tonsils (without measuring the posterior cranial fossa at all).
While a small posterior fossa can cause the cerebellar tonsils to prolapse, there are many conditions that can also cause the tonsils to herniate. When these pathological (causal/attributing) factors go untreated and are allowed to continue pushing/pulling the cerebellar tonsils downward, the brain fails to become buoyant and the patient is left with an even larger hole for the brain to slump into, once again restricting the flow of cerebrospinal fluid. While the patient may initially get a measure of relief from the decompression allowing the CSF to flow, once the brain drops into the hole, the symptoms resume, and doctors are less likely to admit a FAILED DECOMPRESSION.
[More on Pathological Comorbidities]
A small posterior fossa does not cause a problem unless it pushes the cerebellar tonsils down into the foramen magnum (the hole at the base of the skull), causing a blockage of cerebrospinal fluid. Yet, the size of that herniation is THE ONLY THING that doctors routinely measure when they diagnose a Chiari Malformation. They diagnose according to a criteria that only considers the size and appearance of the cerebellar tonsils (without measuring the posterior cranial fossa at all).
✅ Are the cerebellar tonsils herniated by at least 3-5mm?
✅ Are the cerebellar tonsils pointy enough?
While a small posterior fossa can cause the cerebellar tonsils to prolapse, there are many conditions that can also cause the tonsils to herniate. When these pathological (causal/attributing) factors go untreated and are allowed to continue pushing/pulling the cerebellar tonsils downward, the brain fails to become buoyant and the patient is left with an even larger hole for the brain to slump into, once again restricting the flow of cerebrospinal fluid. While the patient may initially get a measure of relief from the decompression allowing the CSF to flow, once the brain drops into the hole, the symptoms resume, and doctors are less likely to admit a FAILED DECOMPRESSION.
[More on Pathological Comorbidities]
Intracranial HYPERtension (IH) headaches tend to be worsened by lying down, so patients often wake up with a headache that gets better after being upright.
[Read More]
[Read More]
Low intracranial pressure (usually associated with CSF leaks) tends to be worse when upright (immediately or over time) and relieved by laying supine.
[Read More]
[Read More]
Craniocervical Instability involves a problem in how the skull is relating to the upper neck vertebrae (C1 or C1/C2), creating a problem in flexion and extension.
[Read More]
[Read More]
Atlantoaxial Instability involves a problem in how the C1 (atlas) and C2 (axis), are relating to one another, creating a problem when rotating head from side to side.
[Discussed in the CCI Article]
[Discussed in the CCI Article]
Basilar Invagination (BI) is a sign of Cranial Settling, where the skull is no longer being properly supported by the neck, and the skull is consequentially dropping along with it's contents.
[Discussed in the CCI Article]
[Discussed in the CCI Article]
©
2007 - 2025
RocketTheme LLC