 Once diagnosed, you will usually be referred to a specialist (not a Chiari Specialist, but an everyday, run-of-the-mill neurologist or neurosurgeon). They tend to come in one of two types: Either they are very passive and just want to wait and see how bad it gets, or they are very pro-surgery and while they will still usually give you a 50% chance of helping your symptoms, they will tell you how decompression surgery really is your best option. Both are problematic.
Once diagnosed, you will usually be referred to a specialist (not a Chiari Specialist, but an everyday, run-of-the-mill neurologist or neurosurgeon). They tend to come in one of two types: Either they are very passive and just want to wait and see how bad it gets, or they are very pro-surgery and while they will still usually give you a 50% chance of helping your symptoms, they will tell you how decompression surgery really is your best option. Both are problematic.
FOR THE ASYMPTOMATIC CHIARIAN:
Without a doubt, the passive approach is by far the best plan of action for the asymptomatic Chiari patient. Approximately 30% of those with a Chiari 1 malformation can go their entire lives without having symptoms (in fact, many remain undiagnosed and don’t even know they have it because they have no symptoms).[1] The Chiari is often discovered while looking for something else entirely and is therefore considered an “Incidental Finding.” While there is a chance that the Chiarian will become symptomatic one day, the risks of surgical complications exceed the potential benefit on something that has not and might not ever affect their life.
FOR THE SYMPTOMATIC CHIARIAN:
If the Chiarian is symptomatic, however, “Decompression Surgery is the only treatment available [at this time] to correct functional disturbances or halt the progression of damage to the central nervous system. Most individuals who have surgery see a reduction in their symptoms and/or prolonged periods of relative stability. More than one surgery may be needed to treat the condition.”[2] Despite the reasons for haste however, we do recommend slowing down and making sure that adequate testing is done to ensure that the Chiari is a “Congenital Chiari” formed only by a small posterior fossa, with no other etiological/pathological co-factors that could make it an “Acquired Chiari Malformation.” If not identified and addressed, these etiological/pathological co-factors can cause complications and even lead to a failed decompression surgery. (Note: most are told at diagnosis that it is a “congenital defect.” However, that is usually a presumption on their part, stemming from a lack of knowledge of Chiari and its comorbidities, and them giving too much credence to the paragraph or two on Chiari malformations in their medical school textbooks. That is not the reality that many are dealing with; so, testing is imperative!)
TESTING:
If you have been diagnosed with a Chiari malformation or a tonsillar ectopia (regardless of the size of tonsillar descent), you should have the following tests/images done.
1. A sleep study to check for Sleep Apnea.
• Central Sleep Apnea (CSA) is more common with Chiari, especially when there has been damage to the brainstem or Vagus Nerve.
• Obstructive Sleep Apnea (OSA) is commonly linked with obesity in the general population, it is also very common amongst those with Connective Tissue Disorders (such as Ehler’s-Danlos Syndrome).
• Both CSA and OSA can be present in the Chiarian with a Connective Tissue Disorder. When both are causing apnea, it becomes known as “Complex Sleep Apnea.”
• Sleep Apnea, regardless of the type, is a common “killer” amongst Chiarians.
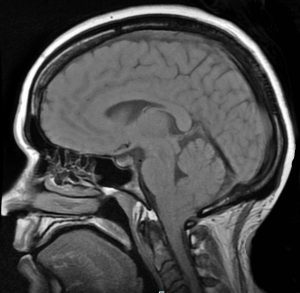
 2. A brain and full spine MRI (upright recommended) with and without contrast.
2. A brain and full spine MRI (upright recommended) with and without contrast.
What they should be looking for in these MRIs:
a) Do you have a syrinx (Syringomyelia or Syringobulbia)?
• If you have either, that is proof that the blockage of CSF is significant enough to cause these potentially serious complications.
b) Is any part of your brainstem below the foramen magnum?
• If it is, you have a variant of Type 1, known as a Chiari 1.5[3] or Type 2, both indicate that there is something else going on causing the brainstem to herniate along with the cerebellar tonsils.
c) Do you have a cyst/tumor causing increased intracranial pressure that is pushing the cerebellar tonsils down?
• If you have either, and they are operable, there is a chance that surgically removing it could decrease the intracranial pressure and allow the cerebellar tonsils (and brainstem if it is below the foramen magnum at all) to go to proper position. Furthermore, if the cyst/tumor is not addressed before, during, or soon after decompression surgery, the chances of your tonsils herniating again after decompression are high.[4]
d) Do you have Hydrocephalus causing increased intracranial pressure that is pushing the cerebellar tonsils down?
• If you do, there is a chance that the placement of a Ventriculoperitoneal Shunt could decrease the intracranial pressure enough to allow the cerebellar tonsils (and brainstem if it is below the foramen magnum at all) to go to their proper position. Furthermore, if the Hydrocephalus is not addressed before, during, or soon after decompression surgery, the chances of your tonsils herniating again after decompression are high.[5]
e) Do you have signs/symptoms of Idiopathic Intracranial Hypertension (often shows as excessive fluid above the lateral ventricles, with small, “slit-like” lateral ventricles; usually accompanied by Papilledema and/or Empty Sella Syndrome), which can cause enough cranial pressure that it can push your cerebellar tonsils down?
• If you do, there is a chance that a prescription for Diamox or Topamax, or the surgical placement of a Ventriculoperitoneal Shunt, could reduce the pressure enough to allow the cerebellar tonsils (and brainstem if it is below the foramen magnum at all) to go into proper position. Studies exist both in favor of shunting first and doing the decompression first; there are documented cases where unresolved IH has led to failed decompression surgeries, while other cases attribute a Chiari decompression as being that which resolved IH symptoms.[6/7]
f) Do you have signs/symptoms of Tethered Cord Syndrome that could be pulling on the spine from below?
• If you do, there is a chance that a less invasive surgery known as a Tethered Cord Release, could stop the downward pulling of the spinal cord and allow the cerebellar tonsils (and brainstem if it is below the foramen magnum at all) to go into proper position. Furthermore, if the Tethered Cord is not addressed before, during, or soon after decompression surgery, the chances of your tonsils herniating again after decompression are high. (Note: not all Tethered Cords are easily visible by MRI, when they are not visible, it is called Occult Tethered Cord (OTC) and surgery on a OTC remains controversial.)[8]
g) Do you have signs/symptoms of Intracranial Hypotension (CSF Leak) that could be pulling or creating a suctioning effect from below?
• If you do, there is a chance that a less invasive blood patch or a Dural Tear Repair Surgery, could stop the downward pulling/suctioning effect on the spinal cord and allow the cerebellar tonsils (and brainstem if it is below the foramen magnum at all) to go into proper position. Furthermore, if the leak(s) are not addressed before, during, or soon after decompression surgery, the chances of your tonsils herniating again after decompression are high. (Note: not all leaks are easily visible by MRI.)[9]
h) Do you have signs of Spina Bifida (Myelomeningocele, Meningocele, or Spina Bifida Occulta)?
• While it is important to know if any of these exist, a Myelomeningocele would put you at an increased risk of having a Chiari Type 2. While all Chiari Malformations with a Myelomeningocele do not meet the standards for Type 2, 90% of those with a Myelomeningocele have a Chiari Type 2. Most neurosurgeons will not perform a decompression on someone with a Myelomeningocele because of the risk of further complications.[10]
i) Do you have signs/symptoms of disc degeneration problems and/or stenosis, especially in the cervical spine where it can damage the Vagus Nerve?
• If you do, these could be another sign of a connective tissues disorder. If you have a syrinx above a herniated/bulging disc, there is a good chance that the disc is attributing to it. Herniated/bulging discs in the cervical spine can be quite troublesome. They can usually be addressed by a second procedure called an Anterior Cervical Discectomy and Fusion (ACDF), but if there are multiple cervical problems and Craniocervical Instability, some surgeons will opt to do a fusion at the time of decompression.[11]
j) Do you have signs and symptoms of a cervicomedullary syndrome[12], which are often the result of Craniocervical Instability (CCI), Atlantoaxial Instability (AAI), or both. (CCI and AAI can be confirmed with: An upright c-spine MRI with flexion, extension, and neutral views or a 3D cervical CT with rotational views.)
• CCI/AAI can produce many of the same symptoms as Chiari 1 malformation, including occipital or craniocervical junction headaches made worse by Valsalva maneuvers. It has been theorized that CCI/AAI may also be capable of causing or worsening a herniation of the cerebellar tonsils, and it has been demonstrated that CCI can cause ventral brainstem compression and deformative stress injury to the brainstem.[13] Failure to diagnose and treat CCI before or along with decompression has also been linked to decompression failure. CCI and AAI, while rare in the general population, are relatively common in patients with HDCT’s (Heritable Disorders of Connective Tissue), such as Ehlers-Danlos Syndrome. CCI, when identified to be the root cause of significant symptoms, can be treated conservatively, and in the short term, with the use of a hard-cervical collar, physical therapy and, possibly, traction. More permanent treatment in the form of a fusion and stabilization surgery (fusing the occiput to C1, C2, and sometimes additional vertebrae).[12/13]
3. A preliminary check for connective tissue disorder (especially Ehler’s-Danlos Syndrome). If preliminary results indicate the presence of a connective tissue disorder, genetic testing should be done to rule out more serious types.
IF NONE OF THESE PROBLEMS APPEAR TO EXIST:
Some doctors and patients prefer to wait and just treat the symptoms medically. That is your choice to make and you should never let anyone try to bully you or manipulate you into having surgery or not; although it is important to know that statistics show that those who have had a shorter duration of onset of symptoms and surgery tend to have a better surgical outcome.[14]
Statistics show that 80% of decompressed patients report some relief from some of their symptoms; headaches are the most commonly reported symptom to gain relief (81%).
Most surgeons will give a 50% chance of relieving each symptom individually, with the exception of pain associated with damaged nerves.
While some surgeons prefer a conservative approach to surgery such as a “bone only” decompression or a “Minimally Invasive Subpial Tonsillectomy,”[15] a full decompression usually consists of:
♦ Craniectomy: removal of part of the sub-occipital skull.
♦ Laminectomy of C1 (and sometimes C2): removal of the lamina from the vertebra.
♦ Duraplasty: opening of the dura (the outermost membrane enveloping the brain and spinal cord) and patching it so there is more room.
♦ Cerebellar Tonsillectomy: removal/cauterization of the cerebellar tonsils.
IS DECOMPRESSION SURGERY A CURE FOR A CHIARI MALFORMATION?
There is a fundamental problem with the question and what many neurologists and neurosurgeons believe about decompression surgery. For the patient, the symptoms are synonymous with the condition. If we continue to struggle living our lives because of these symptoms, having a doctor that refuses to validate that struggle, can add insult to injury. Decompression surgery should NEVER be considered a cure to the symptoms of a Chiari malformation, it is merely the only treatment available [at this time] to correct functional disturbances or halt the progression of damage to the central nervous system. The likelihood of continued symptoms is almost absolute, Decompression is only a means of reestablishing the flow of CSF between the brain and spinal canal (which is imperative). Once flow is restored, there should be some relief from many of the symptoms. Complications such as Syringomyelia should be reduced or resolved, so the possibility of paralysis is significantly reduced. With as bad as the pain and symptoms are, it really can get worse if left untreated. Finding a specialist that is not only experienced with decompression surgeries, but who fully understands the correlation and treatment of etiological/pathological co-factors and co-morbid conditions, substantially increases the likelihood of a positive surgical outcome.
[wpedon id=”4396″ align=”center”]
References:
1 Elster, A D, and M Y Chen. “Chiari I Malformations: Clinical and Radiologic Reappraisal.”Radiology., U.S. National Library of Medicine, May 1992, <www.ncbi.nlm.nih.gov/pubmed/1561334>.
2 “Chiari Malformation Fact Sheet.” National Institute of Neurological Disorders and Stroke, U.S. Department of Health and Human Services, June 2017, <www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Chiari-Malformation-Fact-Sheet>.
3 Kim, In-Kyeong, et al. “Chiari 1.5 Malformation : An Advanced Form of Chiari I Malformation.”Journal of Korean Neurosurgical Society, The Korean Neurosurgical Society, Oct. 2010, <www.ncbi.nlm.nih.gov/pmc/articles/PMC2982921/>.
4 Wang, J, et al. “Acquired Chiari Malformation and Syringomyelia Secondary to Space-Occupying Lesions: A Systematic Review.” World Neurosurgery., U.S. National Library of Medicine, Feb. 2017, <www.ncbi.nlm.nih.gov/pubmed/27894943>.
5 Graham, A, et al. “An Unusual Cause of Neck Pain: Acquired Chiari Malformation Leading to Brainstem Herniation and Death.” The Journal of Emergency Medicine., U.S. National Library of Medicine, Dec. 2012, <www.ncbi.nlm.nih.gov/pubmed/21215551>.
6 Fagan, L H, et al. “The Chiari Pseudotumor Cerebri Syndrome: Symptom Recurrence after Decompressive Surgery for Chiari Malformation Type I.” Pediatric Neurosurgery., U.S. National Library of Medicine, 2006, <www.ncbi.nlm.nih.gov/pubmed/16357496>.
7 Park, Michael S., et al. “Coexistent Chiari Malformation and Idiopathic Intracranial Hypertension: Which Should Be Treated First?- Case Report and Review.” JSM Neurosurg Spine, vol. 2, no. 3, ser. 1025, 20 Mar. 2014. 1025, <www.jscimedcentral.com/Neurosurgery/neurosurgery-2-1025.pdf>.
8 Milhorat, T H, et al. “Association of Chiari Malformation Type I and Tethered Cord Syndrome: Preliminary Results of Sectioning Filum Terminale.” Surgical Neurology., U.S. National Library of Medicine, July 2009, <www.ncbi.nlm.nih.gov/pubmed/19559924>.
9 Atkinson, J L, et al. “Acquired Chiari I Malformation Secondary to Spontaneous Spinal Cerebrospinal Fluid Leakage and Chronic Intracranial Hypotension Syndrome in Seven Cases.” Journal of Neurosurgery., U.S. National Library of Medicine, Feb. 1998, <www.ncbi.nlm.nih.gov/pubmed/9452230>.
10 Vandertop, William P., et al. Surgical Decompression for Symptomatic Chiari II Malformation in Neonates with Myelomeningocele. Oct. 1992, <www.thejns.org/doi/abs/10.3171/jns.1992.77.4.0541>.
11 Dahdaleh, Nader S., and Arnold H. Menezes. Incomplete Lateral Medullary Syndrome in a Patient with Chiari Malformation Type I Presenting with Combined Trigeminal and Vagal Nerve Dysfunction. 2008, <www.thejns.org/doi/pdf/10.3171/PED.2008.2.10.250>.
12 Henderson, Fraser C., et al. “Neurological and Spinal Manifestations of the Ehlers–Danlos Syndromes.” American Journal of Medical Genetics Part C: Seminars in Medical Genetics, 21 Feb. 2017, <www.onlinelibrary.wiley.com/doi/10.1002/ajmg.c.31549/full>.
13 Henderson, FC, et al. “Deformative Stress Associated with an Abnormal Clivo-Axial Angle: A Finite Element Analysis.” Surgical Neurology International, 16 July 2010, <www.europepmc.org/articles/PMC2940090/>.
14 Ma, J, et al. “Cerebellar Tonsillectomy with Suboccipital Decompression and Duraplasty by Small Incision for Chiari I Malformation (with Syringomyelia): Long Term Follow-up of 76 Surgically Treated Cases.” Turkish Neurosurgery., U.S. National Library of Medicine, 2012, <www.ncbi.nlm.nih.gov/pubmed/22664992>.
15 Beecher, Jeffrey S., et al. “Minimally Invasive Subpial Tonsillectomy for Chiari I Decompression.” Acta Neurochirurgica, Springer Vienna, 5 July 2016, <www.ncbi.nlm.nih.gov/pmc/articles/PMC4980444/>.
 Chiari Malformation Vs. Arnold Chiari Malformation
Chiari Malformation Vs. Arnold Chiari Malformation But to look at the full history of what became known as a Chiari Malformation, we can begin by looking at the research of a German pathologist, named Theodor Langhans. In his research in 1881 (a decade before Hans Chiari conducted his research on what became known as a Chiari Malformation), while looking at syringomyelia (“a cavity created in the spinal cord”), he noted a “change in the cerebellar cavity.” Upon dissection of the cerebellum, he described the cerebellar tonsils as “two symmetrical pyramidal tumors,” pushing the brainstem forward.[4] In fact, the other noted researchers: Nicholas Tulp (1593–1674), John Cleland (1835–1925), and Julius Arnold (1835–1915), all centered on the hindbrain hernia [herniation] without speculation as to its etiology/pathology. It is said that “many of the English translations of Chiari’s work contain inaccuracies.” But note that Chiari’s first paper was on “ectopia of cerebellar tissue,” and that he went on to define Type 1 as showing, “elongation of the tonsils and medial parts of the inferior lobes of the cerebellum into cone shaped projections, which accompany the medulla oblongata into the spinal canal.”[5] Which sounds like what is now known to be a Chiari 1.5. Much later, in 1938, at a time when the posterior fossa decompression became the popular surgical treatment for a Chiari Malformation, a Chiari 2 patient “underwent posterior fossa exploration with the authors not considering hindbrain herniation in their differential. Penfield and Coburn later stated that: ‘In retrospect it seems that we should have suspected the Arnold-Chiari malformation. Instead, a suboccipital craniotomy was carried out…” So even the early neurosurgeons seeking to perfect their surgical treatment felt that it was a mistake to concentrate on the posterior fossa and not take into account etiologies of the hindbrain herniation. That mistake is still going on 80 years later.[6]
But to look at the full history of what became known as a Chiari Malformation, we can begin by looking at the research of a German pathologist, named Theodor Langhans. In his research in 1881 (a decade before Hans Chiari conducted his research on what became known as a Chiari Malformation), while looking at syringomyelia (“a cavity created in the spinal cord”), he noted a “change in the cerebellar cavity.” Upon dissection of the cerebellum, he described the cerebellar tonsils as “two symmetrical pyramidal tumors,” pushing the brainstem forward.[4] In fact, the other noted researchers: Nicholas Tulp (1593–1674), John Cleland (1835–1925), and Julius Arnold (1835–1915), all centered on the hindbrain hernia [herniation] without speculation as to its etiology/pathology. It is said that “many of the English translations of Chiari’s work contain inaccuracies.” But note that Chiari’s first paper was on “ectopia of cerebellar tissue,” and that he went on to define Type 1 as showing, “elongation of the tonsils and medial parts of the inferior lobes of the cerebellum into cone shaped projections, which accompany the medulla oblongata into the spinal canal.”[5] Which sounds like what is now known to be a Chiari 1.5. Much later, in 1938, at a time when the posterior fossa decompression became the popular surgical treatment for a Chiari Malformation, a Chiari 2 patient “underwent posterior fossa exploration with the authors not considering hindbrain herniation in their differential. Penfield and Coburn later stated that: ‘In retrospect it seems that we should have suspected the Arnold-Chiari malformation. Instead, a suboccipital craniotomy was carried out…” So even the early neurosurgeons seeking to perfect their surgical treatment felt that it was a mistake to concentrate on the posterior fossa and not take into account etiologies of the hindbrain herniation. That mistake is still going on 80 years later.[6] Unfortunately it leaves most of us with failed decompressions, fighting with our neurosurgeons that “something is still wrong.” These neurosurgeons look at their post-operative checklist and see that they successfully did everything surgically required in their out-of-date textbooks:
Unfortunately it leaves most of us with failed decompressions, fighting with our neurosurgeons that “something is still wrong.” These neurosurgeons look at their post-operative checklist and see that they successfully did everything surgically required in their out-of-date textbooks:






 Empowering With Knowledge!
Empowering With Knowledge!  be, but if we continue to see all that we can do and not just what we cannot do, we can dare to dream again! We are all multifaceted human beings with broad gifts and talents. We might not be the athletes we once aspired to be, but that says nothing of our strength. We all have the potential to change the world around us! You might be an artist that hasn’t practiced your art in years – start practicing again! You might have always thought about writing books, but because of your diminished hope for the future, you haven’t written in years – pick up a pen and start writing again! The only way to ever know your true potential is to try and try again! Dare to dream again!
be, but if we continue to see all that we can do and not just what we cannot do, we can dare to dream again! We are all multifaceted human beings with broad gifts and talents. We might not be the athletes we once aspired to be, but that says nothing of our strength. We all have the potential to change the world around us! You might be an artist that hasn’t practiced your art in years – start practicing again! You might have always thought about writing books, but because of your diminished hope for the future, you haven’t written in years – pick up a pen and start writing again! The only way to ever know your true potential is to try and try again! Dare to dream again! 


 Once diagnosed, you will usually be referred to a specialist (not a Chiari Specialist, but an everyday, run-of-the-mill neurologist or neurosurgeon). They tend to come in one of two types: Either they are very passive and just want to wait and see how bad it gets, or they are very pro-surgery and while they will still usually give you a 50% chance of helping your symptoms, they will tell you how decompression surgery really is your best option. Both are problematic.
Once diagnosed, you will usually be referred to a specialist (not a Chiari Specialist, but an everyday, run-of-the-mill neurologist or neurosurgeon). They tend to come in one of two types: Either they are very passive and just want to wait and see how bad it gets, or they are very pro-surgery and while they will still usually give you a 50% chance of helping your symptoms, they will tell you how decompression surgery really is your best option. Both are problematic.